
The Consumer Engagement Reference Architecture (CERA) strategically combines Microsoft's existing and emerging consumer properties. CERA brings several unique advantages to health plans seeking to engage consumers in their health, gain a competitive advantage, and elevate their perception to trusted health advocate in the eyes of their customers.
Scale and Extend High Impact Health Management Services
CERA gives health plans an unprecedented capacity to scale and extend their labor-intensive care and health management service models to achieve greater economies of scale and a better bottom line. CERA can scale the impact of health management teams by virtualzing and automating the business and care processes that matter most when it comes to improving personal health and reducing medical costs – the participatory processes that engage consumers actively with their health and connect them to their live or virtual coaches. When engaged consumers stay connected with the coaches they trust, most are able to make and sustain the incremental health behavior changes that, when repeated, lead to healthier lifestyles and reduced health risks and medical costs.
By further extending the reach of coaching into the channels and devices that consumers prefer, health management teams can more easily connect and stay connected with consumers to ensure they develop self-efficacy skills and achieve their healthier lifestyle goals.
While readiness and intent to improve health behaviors and personally relevant health information are necessary for consumers to improve their health behaviors, neither of these alone are typically sufficient to overcome the powerful inertia of existing unhealthy habits. Indeed, successfully improving health behaviors typically requires systematic and interpersonal interactions with trusted advisors – like coaches, care management nurses, and personal physicians – that work collaboratively with consumers to set and achieve goals.
By making these interactions "normal" experiences within the consumer's online world, CERA's technology-generated “moments of participation” can repeatedly nudge consumers to stay engaged and continuously make small changes that they can live with over and over. By combining nudge economics with personalized moments of participation, health plans can empower consumers to turn their good intentions into healthier lives and lower medical costs over their lifetime.
Business Imperatives for Health plans
Health plans are under unprecedented pressure to both improve the health and quality outcomes of members, and also to mitigate the spiraling costs of health insurance that’s draining the resources of employers and raising the ranks of the uninsured. Despite the recent moderation in health care spending growth from double-digit to single-digit levels, medical cost growth still outpaces GDP growth by two to three percent. As a result, healthcare costs continue to put U.S. corporations at a competitive disadvantage with foreign companies.
To address these market demands, health plan executives are deploying three transformational levers to transform the current procedural reimbursement model into a shared accountability model where plans, providers, and consumers have the aligned incentives and the actionable information they need to positively impact the quality and affordability of care.
Transformational Levers
Health plans are introducing innovative, value-based benefit designs that are transparent and align incentives for all stakeholders: payers, consumers, and providers. These new designs shift accountability and incentives to consumers through higher coinsurance, CO-payments, and/or deductibles, and empower them with the self-efficacy tools they need to become more active consumers of healthcare.
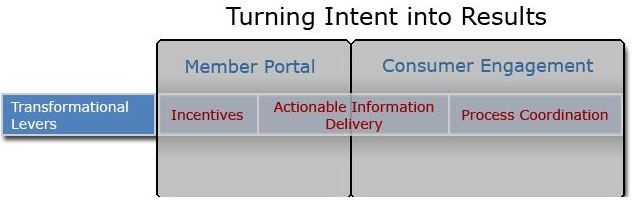
Figure 1. Transformation levers
Actionable information delivery
Target and engage consumers in comprehensive health management services that range from preventive health and pre-onset disease management to efficient and effective self-management and treatment of acute and chronic diseases. To do so, this new model holistically combines wellness, 24/7 nurse channels, preference-sensitive conditions, complex case management, and care coordination. It also provides a continuing and increasing focus on disease management, wellness, and innovative benefit products that identify and reward early participation in programs that increase wellness and improve long-term health
Ecosystem process coordination
Support cross-organizational collaborative processes to promote a safer, more effective, and interconnected health care system. Our current delivery system was never designed to manage chronic diseases (for example, diabetes, cardiovascular diseases, asthma) that consume 75 percent of our healthcare spending – and it shows when patients, providers, and health plans feel like they are working off different pages and we experience care that is evidence-based only slightly more than 50 percent of the time. Instead, online communications, the sharing of information and insights, and the coordination of workflow across the health-value web will be the enabler of the personalized health model by promoting high-quality decisions for consumers and medical professionals alike.
Engaging consumers in their health
But spiraling medical cost growth is firmly rooted in our personal choices and health behaviors. Our unhealthy behaviors such as neglecting health screening, smoking, unhealthy diets, lack of physical activity, non-adherence to prescribed care plans, sleep deprivation, and alcohol misuse lead to chronic diseases – which account for more than 75 percent of medical costs. Indeed, personal health behavior is the single greatest influence on chronic disease death, and the medical cost growth trend that has defied both market and regulatory interventions.
This means that the best efforts of health plans to put the brakes on the growth in medical costs will have limited impact until consumers take their feet off their unhealthy behavior gas pedals and become actively engaged in their health. Consumers will need to focus more on improving, managing, and monitoring their personal health behaviors, lifestyles, and chronic diseases than they focus today on recovering from their illnesses and injuries. Becoming active healthcare consumers means that they will need to think less about "getting care" from the medical system and think more about "taking care" into their own hands and staying as healthy as possible. They will need to assimilate information, skills, and confidence to collaborate with, rather than taking orders from, medical professionals. And they will need to assume responsibility for contributing and transmitting critical clinical information to support their physicians' diagnostic and treatment decisions.
Besides accounting for 75 percent of medical costs, personal health behavior is also the single most prominent domain of influence over preventable deaths in the United States. According to the CDC, approximately 40 percent of deaths are caused by behavior patterns that could be modified by preventive interventions, like quitting tobacco use, eating nutritious foods (only 25 percent of US adults eat the recommended five or more servings of fruits and vegetables a day), being physically active (more than 60 percent of U.S. adults do not exercise enough), and not overusing alcohol.
It gets worse. Because it’s our poor health habits of today that are guaranteeing the growth of medical costs and deaths related to chronic disease for coming generations. The rising prevalence of chronic conditions — particularly diabetes and heart disease – is now being fueled by the epidemic of obesity, with 64 percent of Americans now overweight and 30 percent classified as obese. This means that in the decade to come, more, not fewer, Americans will be handed the diagnosis of diabetes, hypertension, hyperlipidemia (high cholesterol), heart disease, stroke, and some forms of cancer. Our obesity epidemic has become sufficiently widespread that obesity is now in line to be the next public health epidemic and actually reverse the 25 years of life expectancy we gained last century as a result of public health achievements in immunization, infection control, and workplace safety.
The implication for health plans is clear and sobering: improving health, quality, and affordability boils down to improving the behavioral choices of not only patients with chronic, costly conditions, but also those in the population who are now at risk for developing a chronic condition.
Embrace personal consumer technologies
For health plans to successfully get and keep consumers engaged as active participants in their health and health decisions, health plans will first need to need to understand and embrace the established and emerging technologies that consumers are using at home, at work, and on the go. This requires innovative and out of the box thinking for health plans (transformation) that, historically, have built their businesses on a transaction-processing infrastructure.
This means health plans will need to design and implement personal health enablement software that activates and engages consumers to change their personal health habits alongside their legacy transaction, customer relations management (CRM), and medical management systems. Unlike data-driven transactions, personal health enablement software will need to promote incremental personal health behavior changes in the direction of better self-management and better health habits. More specifically, personal health enablement software will need to:
Standing in the way of the health plan's efforts to engage consumers in their healthcare are two non-trivial barriers. First, the health management services with the greatest potential to get and keep consumers engaged as active participants in their health and health decisions rely on processes that are highly complex and largely people-driven. Second, engaging consumers is much harder than it looks and needs to be lifetime mindset rather than a "once-and-done" occurrence.
Health management services – customer service, care management, and lifestyle coaching – are complex, costly, and difficult to scale for several good reasons. Wellness and care-management nurses are in short supply and are commanding higher compensation and concessions. Turnover is high and costly. And consumer-centered health management is complex because it spans a very broad continuum that extends across multiple domains – from wellness management and authorizations to catastrophic case management and chronic, unstable disease management.
Furthermore, the data and people needed for health management are also disparate, scattered, and span throughout the ecosystem. As a result, every stakeholder holds pieces of important data – including the payer, multiple providers, the patient, and even family members. This multidisciplinary nature of wellness management, combined with the complexities of personal health that requires the communications and coaching skills of medical professionals, make wellness management services extremely difficult to scale and automate.
Lastly, health management services scale poorly because the processes are largely people-driven, highly collaborative, and they run end-to-end across the workplace, the home, and company boundaries. Unlike administrative transactions that run machine-to-machine, the processes that reduce medical costs and risks are much more difficult to manage and automate because they are non-routine, unstructured, and rely on the insights, coordination, and actions taken by people.
Wellness and care management processes, tasks, disparate data, and workflows cross the boundaries of productivity software, care management software, and multiple organizations across the entire healthcare ecosystem. The implication of this broad continuum challenge means there will never be a single commercial solution that can meet the full continuum of health management needs for the health plan enterprise. Any automation solution, regardless of whether it’s a packaged application or developed in-house, will require extensive integration with existing back-end systems, cross-organizational information system integration, and cross-organizational ("community") workflow.
Health plans and worldwide ministries of health have a business imperative to help members develop self-efficacy skills and get and stay as healthy as possible to reduce runaway medical costs. In fact, the single best way to improve their bottom line is to keep high-risk members healthy and prevent costly complications and hospitalizations.
Today, employees might sign up online for their health benefits – but after that they are expected to step outside their preferred online experience to a portal to get service, find information, or get tools to help them take better care of themselves and make value-based decisions about their care.
But changing health behavior is complex, takes time, and involves more than, as goes the cliché, "getting the right information to the consumer at the right time and place." Granted, incentives and better information are a good start and consumers need far better information than they have today to make value-based decisions. But information itself is only valuable to the extent that it enables sustainable behavior changes among consumers. And we all know from personal experience that, while information alone may be necessary, information alone has never been sufficient to change our stubborn unhealthy habits for the better. Even knowing what about our health behaviors need to change and why they need to change is seldom enough to change stubborn unhealthy habits like sleep deprivation, overeating, eating the wrong things, under-activity, stress, tobacco, and alcohol use.
Most of us know from experience that behavior change is a complex process that, more often than not, requires systematic interpersonal interactions with trusted advisors – like coaches, care management nurses, and personal physicians – that work collaboratively with each individual to set and achieve goals.
Despite having portals that are fully stocked with state-of-the-art personal health information and tools, health plans are extremely limited in their capacity to “connect” with consumers day-to-day because:
But no matter how available or useful and essential these health information, tools and guidance are, they are unless consumers actually use them. Today, employees might sign up online for their health benefits –but after that they prefer to use the phone because:
And, lastly, consumer engagement is an ongoing day to day process that never ends, not a transaction every month or so. Health plans need to engage consumers and then keep them actively engaged in their health throughout the course of their entire lifetimes.

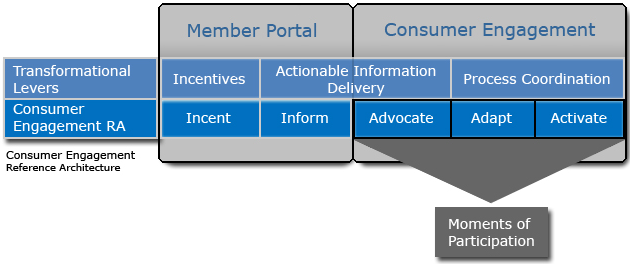
Innovative technologies are needed to support the three key strategies that can enable health plans to overcome these barriers to engaging consumers in their health. These strategies are advocate, adapt, and activate. These technologies must advocate personal health by scaling and extending labor-intense health management processes, adapt multiple health management interfaces to the digital lifestyles and preferences of consumers, and activate members to continually improve their health behaviors and self-manage their conditions.
Technologies must scale and extend health management processes (health coaching and care management processes) into the day-to-day digital lifestyles of members.
Through health management and lifestyle changes, health and healthcare must become joint activities in which both consumers and providers engage, much like the analogy of a coach and a player. The coach provides technical know-how, insights, and encouragement to the player. But, ultimately, it's the player who scores the points that win the game. Healthcare providers and health management coaches have the technical knowledge, but if the patient does not turn intent into action by assimilating those insights and developing the skills to win, neither the coach nor player can win. Coaching requires both human communications and a human connection. Similarly, to help consumers become effective self-caregivers, they need to communicate and connect with the people who will coach them. They need personalized feedback, ongoing communications, actionable insights about their own capabilities and limitations, and they need continuous opportunities to learn needed skills. They need an online "channel" that's familiar to them that they can call when they need advice or encouragement.
By virtualizing and automating the repeatable health management processes and extending the reach of coaching into the channels and devices that consumers prefer, health plans can scale and amplify the productivity, impact, and return of their health management coaches and teams.
Health management interfaces (such as portals, speech, voice, messaging, and devices) must adapt to the digital lifestyles and preferences of consumers by going where consumers are and co-mingling health into the day-to-day context of consumers’ digital lifestyles.
In a world that is increasingly interconnected, always on, and already engaging consumers, health plans must leverage existing consumer technologies and channels to better engage consumers in a way that enables them to change their behavior in the direction of better health. This requires equipping consumers with personal technologies that adapt to their daily digital experiences.
Rather than hoping, "pushing," and waiting for consumers to adapt their lifestyles to service member portals (that today are teeming with great tools and guidance), technologies must meet consumers where they live and work. Incentives, actionable insights and information, trusted guidance, and communications need to be intermingled into the consumers’ preferred interfaces and channels across the home, the workplace, and connected devices.
This "go where consumers are" approach recognizes the reality that consumer engagement in health is not, today, a well-established, natural human behavior looking for a more efficient online marketplace. Consumers, for example, are adopting Amazon, eBay, and Facebook because these online services offer consumers a "better way" than the analog alternatives. With Amazon, for example, consumers can preview, buy, and sell books online from the convenience of their home rather than wandering the aisles of book megastores. With eBay, consumers can buy and sell used items more quickly and efficiently without the inconvenience and cost of want ads or garage sales. Facebook moves the college campus dorm experience of meeting and socializing online and complements in-person meetings and phone calls. When it comes to consumers engaging in their personal health, there are few, if any, "natural" behaviors or processes looking for a better online way.
This is why member portals need to meet consumers where they are at today, not the other way around. Health plans need to adapt their member portals, health coaching, and health management processes as well into the consumer’s established day-to-day online experience (digital lifestyle), not vice versa. If, for example, consumers between the ages of 18 and 28 are using instant messaging, text messaging, cell phones, blogging, watching movies and playing online games at home, health plans will need to co-mingle health engagement interactions into those activities and channels. If consumers between the ages of 29 and 70 are using e-mail, banking online, buying online, and searching for authoritative health information online, then health plans will need to intermingle health engagement interactions into those activities and channels.
Since better day-to-day decisions and sustainable changes in personal heath behaviors are what matter most when it comes to mitigating the spiraling cost of healthcare and the rising prevalence of chronic disease that's fueling those costs, their active participation must be continually renewed to sustain behavior changes. Technology is needed to generate new and personalized "moments of participation" that activate, engage, and keep consumers continually engaged in their health day to day. These moment renew the consumers’ motivation to improve their health behaviors and self-manage their conditions.
These "moments of participation" are polite and personally meaningful interactions that might be with people, software agents, software interfaces, or mobile devices that promote incremental behavior changes in the direction of better personal health behaviors and reduced health risk. Similar to "moments of truth," those few interactions when the customer feels strongly about the outcome, moments of participation engage the consumer emotionally and promote loyalty and the perception of advocacy.
However, unlike moments of truth that usually occur when the consumer initiates contact with the vendor, moments of participation are provided as a service by the vendor to periodically promote new behaviors and systematically reinforce them when they occur.
Moments of participation periodically engage the consumer in conversation, allow consumers to ask for help in their own words, and can seamlessly escalate any issue, along with all documentation, to a live coach or customer service agent in situations that are too complex or personal for automation. By intermingling these participatory interactions into the day-to-day context of the consumers’ analog and digital lifestyle based on their channel preferences, moments of participation become a "normal" part of the consumer's familiar online experience at home, at work, and on the go.
Moments of participation can be designed to:
Employees of an organization may receive an e-mail or be notified using any other mechanism about an upcoming Health Fair, where they can sign up for health and wellness coaching which will help them in improving their health and give them some incentives. Members either go to the health fair or they may decide to sign up for the program online from their office or home.
The first step of engaging with a health and wellness coach is for the members to enroll. This process of enrollment takes few steps to complete and requires the member entering personal information and health risk appraisal (HRA) information.
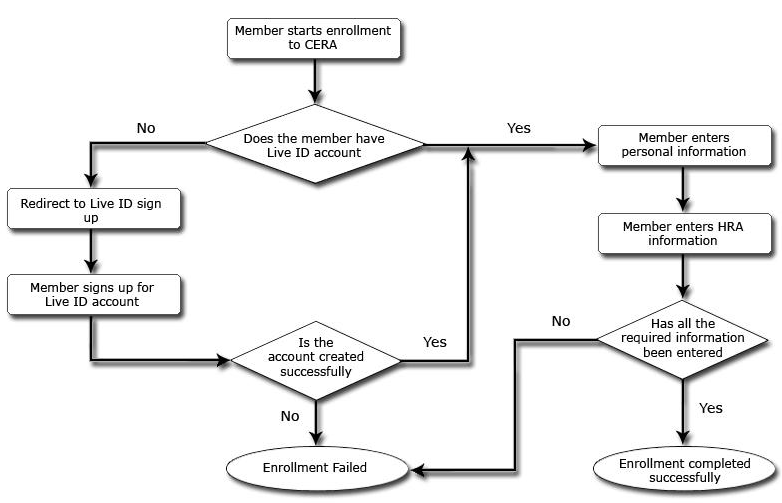
Prior to beginning, the members are required to have a Windows Live ID account as the Live ID is used as the member authentication service. If a member does not have Windows Live ID, then the member is redirected to sign up for Windows Live ID account. With a valid Windows Live ID account the member begins the sign up process.
Windows Live ID is a identity service from Microsoft Windows Live platform providing a unified login service which allows users to log in to many Web sites using one account. It is helps any Web site in providing identity to their users without having to build a complete identity management service from start. Currently many of Microsoft's Web sites such as Hotmail, MSNBC, MSN, Xbox 360's Xbox Live, the .NET Messenger Service, and MSN subscriptions use this service to manage their member identity.
A new user entering a Web site is redirected to the Windows Live ID authentication server to enter their Live ID credentials. These credentials are validated by the Live ID platform and a service ticket issued to the requesting Web site. CERA uses this Live ID service for authenticating members and coaches, who could be logging into the portals from anywhere to receive the coaching and benefits.
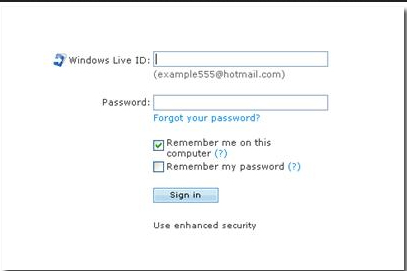
Figure 4. Live ID login
Once the member is successfully logged in, an enrollment wizard helps the member with the process. The members first enter their personal information, followed by their health risk assessment (HRA) information. CERA uses the HRA developed by physicians and experts at the University of Michigan Health Management Research Center. The personalized wellness profile raises health awareness among members and encourages a healthier lifestyle. CERA helps personalize the member’s portal so they can review their wellness profiles at any time and update their profiles with up-to-date information. Once the HRA is completed, a confirmation message on the screen informs the member about the completion and the member also receives a confirmation e-mail informing.
Once the member completes the enrollment process and submits the information, the back-end system assigns a coach to the member. This assignment can be based on the gender, region, medical condition of the member, and so forth. The assigned coach will contact the member for an appointment to validate the HRA.
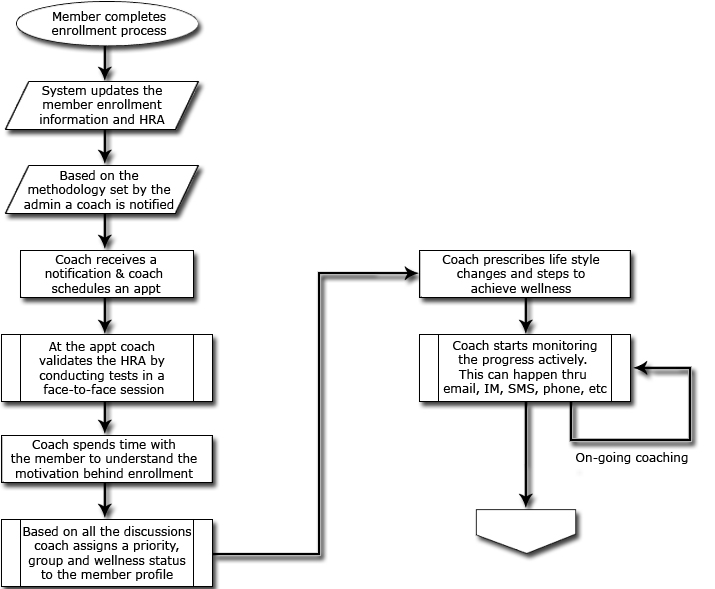
Figure 5. HRA validation flow
During the appointment, the coach notes the height, weight, smoker/non-smoker, blood test, sugar level and other vital information. The coach then spends time understanding the motivation for signing up with the program and member’s goals for the program. Do they want to lose weight, quit smoking, or just become more active? Some members may sign up just to get the benefit of the incentive. Either way this helps the coach in categorizing each member into the proper category and also to devise a plan to help the member. After the appointment, the coach puts the member into a group such a high-risk group, smoking cessation group, weight loss group, or healthy group. Based on the member group, the Health Coach starts creating a plan to help the member and starts communicating regularly using the member portal tools to help the member achieve their wellness goals using prescribed exercises, smoking cessation, weight loss, and so on.
Once the member completes the enrollment process and submits the information, the back-end system assigns a coach to the member. This assignment can be based on the gender, region, medical condition of the member, and so forth. The assigned coach will contact the member for an appointment to validate the HRA.
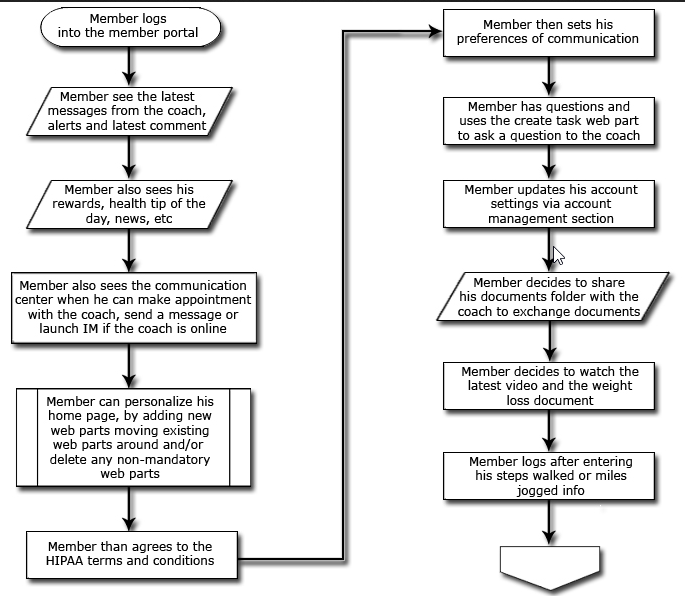
Figure 6. Member portal flow
When the HRA validation is completed, the member receives an e-mail notifying them of the coach assigned to them and welcoming them to the portal. The member logs into the portal which has many Web Parts and also has a Web Part library. The member portal is customizable based on the member’s preferences. Some Web Parts are mandatory and others are optional which the member can easily add or remove from the portal. Mandatory Web Parts are:
In addition there is a library of optional Web Parts:
The portal also has the capability to show if the coach is online.
The Health Coaches get involved once members complete their initial enrollment and submit their health risk assessment documents. The job of the Health Coach is to take a member-centered approach that provides one-to-one support and individualized guidance for behavior and lifestyle change. The Health Coach (a.k.a. “coach”) becomes the member’s key contact and the coach stays involved with the member throughout his or her experience with the health and wellness program.
Health Coaches generally work for a health and wellness program. They may be assigned member “clients” based on a number of criteria such as a member’s demographics, health conditions, and/or health assessment feedback. It is the health coach’s job to initiate and then establish a relationship with the member and to maintain that relationship throughout the member’s experience.
To maximize the Health Coach’s effectiveness a number of tools are provided to the coach. These tools may include a portal, e-mail, secure instant messaging, mobile devices, biometric devices, templates, an electronic health literature and documents library, and so forth. The most useful tool is the Health Coach Portal. The portal is the Health Coach’s “control center”. Within this workspace the Health Coaches have complete visibility into their work schedules, members, member health data, contacts, appointments, requests, alerts, work queues, templates, and other information.
Health coach portal overview
The Health Coaches begin their day in the Health Coach Portal. The Health Coach Portal is comprised of a number of Web Parts that provide specific capabilities and functionality. A number of the Web Parts are mandatory. There are also a number of optional Web Parts to provide enhanced functionality and personalization capabilities that the Health Coach can easily add or remove from the portal. Mandatory Web Parts are:
In addition, there is a library of optional Web Parts:
The portal also has capability to show when the coach’s contacts and members are online.
Health coaching process – “turning information into action”
Health Coaches use the Health Coach Portal as their control center. When they log into their portal they are immediately shown a summary of their work flows and work schedule, new clients assigned, urgent alerts, urgent requests, and open issues.
The Health Coach’s job begins with getting their newly assigned clients up to speed. A key to the success of this process, and the overall coaching program, is for the Health Coach to take action based on the member’s health risk assessment information. To do this, the Health Coach must engage the member in an on-going dialog that provides numerous opportunities for the client to participate in their wellness program.
The diagram depicted below provides a framework for turning health risk assessment information into action. As discussed previously, members are given incentives to transform their behavior. Additional transformation levers for continuous engagement are extended by the Health Coach. The Health Coach provides the member with opportunities to participate in changing their health life style. We call these opportunities “Moments of Participation.”
Collaboration
Engaging with the members is important in achieving results. In addition to information, the coach provides incentives to the customer during the engagement process to motivate the members to complete the steps towards achieving their goals.
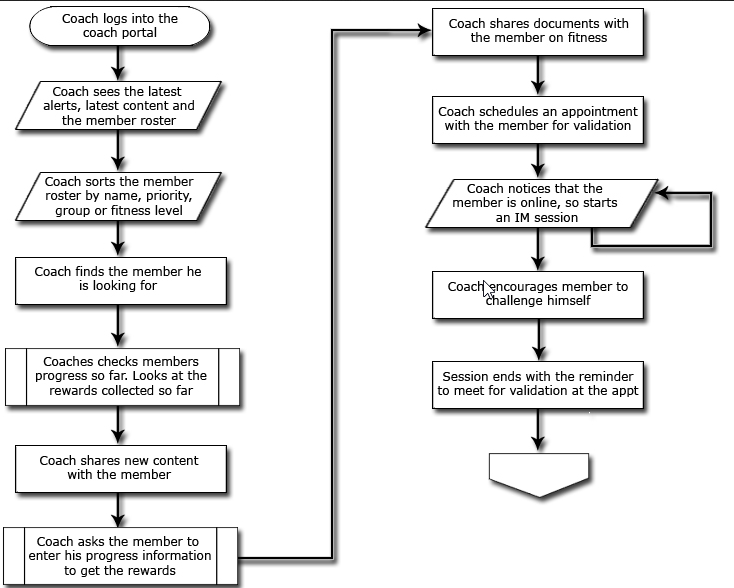
Figure 7. Collaboration flow
Member collaboration with coaches is done primarily through the portal; however the collaboration can also happen using mobile devices and media centers as well. Members use their portal to setup appointments with the coach for HRA validation or monthly visit or to schedule a conf. call. Members also use the CERA platform to chat when the coach is online same time they are online, to log their activity using the automated service agents (ASA), also known as the “bots.” One of the critical elements of collaboration is the ability to share documents. Coaches can collaborate with members by sharing documents with all the members assigned to him/her. In addition, the coach can trigger a workflow to be informed when the members actually view the document. This way, the coach can give incentives to help members actually read the document and follow the instructions to improve their health. The coach sends e-mails to their members about their wellness steps, shares links to new information on health, and sets up appointments for regular check ups. In addition, the coach can see the presence of a member and initiate a chat or a coaching session.
Collaboration activities include:
Collaboration is not limited to presence only, but rather works well even when the member or coach is offline.
To engage with the members and to provide timely guidance requires real-time collaboration between the members and the health coaches. Collaboration should not be limited to simply chatting online, however. It needs to contextual, it needs to be relevant. Collaborating entities need to share data and documents and should be able to discuss the same information through many channels. So the collaboration needed is far beyond a simple e-mail and/or chat technology. To collaborate this extensively requires building a solution that can engage consumers through many channels.
The 2007 Microsoft Office System is a great platform to build collaboration applications. It comes with many capabilities at various levels that facilitate assembling applications. Office System delivers not just the familiar set of Office clients (Word, Excel, InfoPath), but also several key capabilities as services that are delivered on both client applications and also on the server. The collaborative applications that are assembled upon this platform are called Office Business Applications (or OBAs). The high-level capabilities in the 2007 Microsoft Office System are listed below in the table.
|
Capability |
Description |
|
Web site and security framework |
A common framework for creating different kinds of sites e.g. team collaboration sites, intranet portals, internet web sites. |
|
Open XML file formats |
Open formats to represent business documents that can easily be read, transformed and visualized. This enables rich server-side processing of documents in ways that was not possible before. With prior versions of Office, parsing the document using the object model required an instance of the client application. |
|
Extensible UI |
Server-side portal that can be extended by users from a catalog of web parts and the catalog itself can be extended by solutions providers. Client applications with rich capabilities for extensibility through Visual Studio Tools for Office. |
|
Business Data Catalog |
A metadata repository to define business entities stored in back-end data stores, to model relationships between entities, and to define actions permissible on entities. |
|
Enterprise Search |
Surface data from various enterprise sources through search. |
|
Workflow |
Integration with Workflow Foundation to host workflows that represent people-to-people interactions, and that link user interface elements. |
|
Enterprise Content Management |
Manage diverse content, with one topology for web, document and records management. Support for document life-cycle management. |
|
Business Intelligence |
Server-based Excel spreadsheets, plus BI components (dashboards, reports, and web parts) built into the portal and connected to SQL Server Analysis Services. |
|
Communication and Collaboration |
Support for unified communications integrated into the platform |
As listed above, the Microsoft Office platform supports the fundamental building of collaboration, which is unified communications. This is all about connecting people, processes, and information. The ability to surface and share timely information with the members helps them in achieving their wellness goals. For building consumer-engaging solutions such as CERA, the 2007 Microsoft Office Platform provides the capabilities to:
The architecture of a solution that can help in engaging the consumers with a health and wellness program is described in this section. It lays out the logical, functional, and physical architecture of the solution. It also describes the Office platform and Live platform capabilities that are utilized in building this solution.
Logical View
The CERA logical architecture is shown in the figure below. This architecture shows the four tiers, which come together to provide the compelling collaboration application. Typically, application architectures are decomposed into three tiers: presentation, application (or business logic), and data. However the three-tier architecture assumes structured business processes and data, where all requirements are made known during the process of designing and building the system. But engaging with members for wellness and health improvement requires unstructured and informal collaboration. So the solution needs to explicitly account for people-to-people interactions between members and coaches that are essential to get the benefits of this plan. Usually these interactions are not captured by structured processes or traditional business applications, and therefore it is critical to add a fourth tier - the productivity tier – to account for these human interactions.
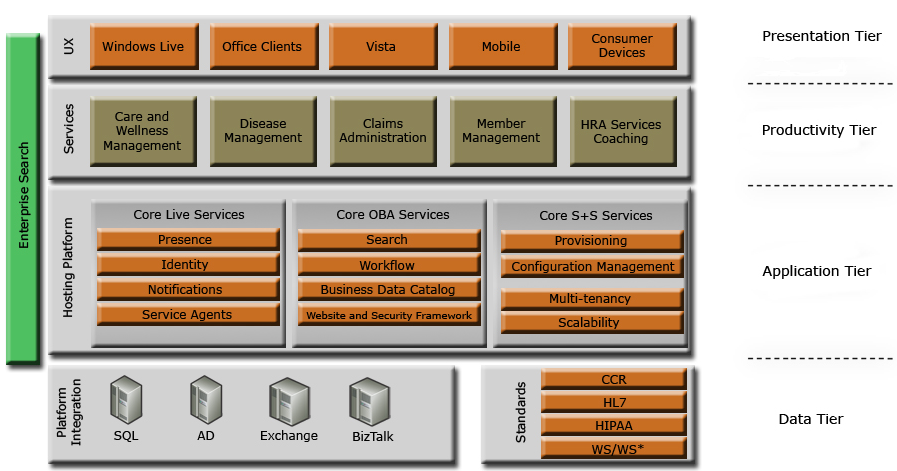
Figure 8. CERA logical view
Let’s look at the various tiers of the architecture and the capabilities they provide which were essential in building CERA.
Data tier
This tier supports much-needed data capabilities for CERA. Member profile information, HRA information, prescriptions, and other information are stored in this tier. This tier also supports the transaction capabilities needed to collaborate with the coach. This is also the tier for integration with LOB applications and third-party applications and services using BizTalk and its HL7 and HIPPA accelerators to exchange standard messages with other applications. Active Directory directory services are used for the identity management of the administrator; whereas Windows Live ID is used for members and coaches.
Application tier
This is business logic and services layer. All core services are provided by this layer which rely on the data from the data tier and enable productivity tier for create workflows, create applications, and so on. This is the layer that supports business process management (BPM) for structured processes. Some of the core capabilities supported by this tier are the presence information, member and coach identity, workflows, and service agents. All of these capabilities play a critical role in enabling the real-time collaboration between members and coaches through e-mail, IM, automated bots, and other means.
Productivity tier
The productivity tier consumes the services and data of the underlying tiers to enable the collaboration. Document management is another area enabled in this tier, as is sharing of information for wellness management. This tier also enables sharing of member information, HRA information and document sharing between the coaches and. Services enabled by underlying tiers enable creation of HRA validation workflow, activity logging, and other collaborative functions.
Presentation tier
This is the tier where information is consumed for collaboration between different users. User experience is provided in this tier to record transactions, to make decisions, and to create and share documents. User experience can be either based on Office clients (InfoPath, SharePoint portals), smart clients, Web browsers, or devices such as Windows Mobile phones.
Functional View
This four-tiered architecture plays a critical role in building a real-time collaboration solution for health and wellness management. Figure 9 shows the architecture of CERA for health plans.
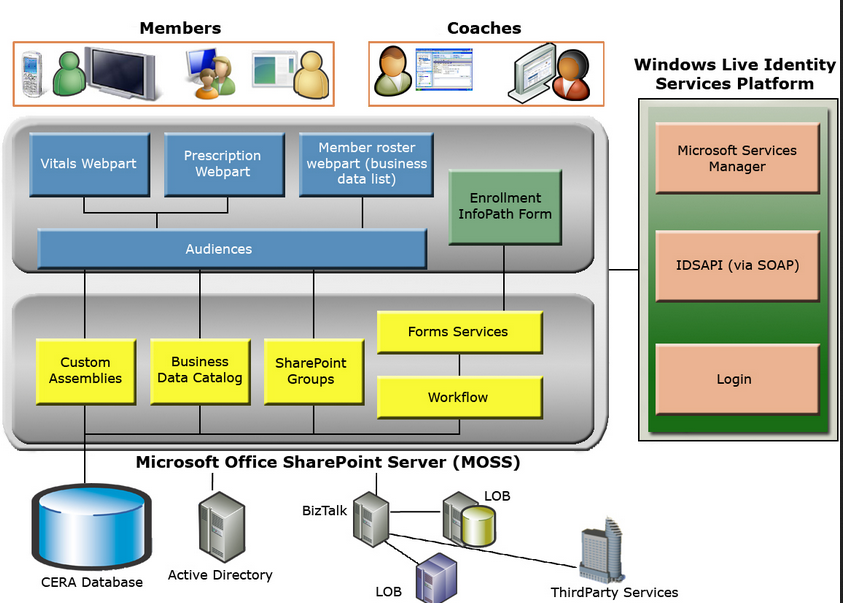
Figure 9. Functional view of CERA
This CERA architecture shows the core capabilities of MOSS used in building this solution. To enable collaboration for wellness management and health coaching, the following fundamental building blocks were used.
Web Parts
Web Parts surface member information, vital information, prescription information, and so on.
Workflow
Workflow capability is used to enable workflows around wellness management.
InfoPath
CERA uses InfoPath forms for designing the enrollment forms and HRA forms. InfoPath provides flexibility in terms of the form display UI (Web, Office, and so on) and supports built-in form validation. In addition, they support custom validation of certain form fields.
InfoPath has been designed to let users design a form once for both the rich client and the browser. When browser compatibility is enabled, not all InfoPath features are available and some will be limited in their functionality in the Web browser. The CERA member enrollment form is designed and is published to the server running InfoPath form services. In CERA, only browser-based InfoPath forms are used, which removes the requirement to have the InfoPath client on the member’s computer.
InfoPath provides a level of validation for the data entered through the browser, ensuring that the quality of the data submitted by a form is the same, regardless of the client that has been used to fill it out. In other words, for “design once” forms, the XML schema validation, rules, conditional formatting, and business logic apply the same way for both rich and browser forms.
Critical features of InfoPath are:
The CERA client can be either the browser or a mobile device. Even though it was not demonstrated, the architecture does not limit use of other clients such as an Office client (such as Outlook), a smart client, or a media center client. In all the cases, the CERA platform will support the requirements for collaboration and information sharing. The next sections walk through the steps of building CERA.
Building CERA involved many steps and this section will walk briefly though these steps.
1. Design the database that holds member, coach, and HRA information for health and wellness coaching.
2. Integrate with Live ID for member and coach identity management.
3. Create the SharePoint groups, for example Member group, Coach group, and Admin group.
4. Create the custom assemblies. These are .NET applications that will enable custom Web Parts such as vitals and prescription.
5. Create the BDC metadata to surface information from the database such as member profiles, prescription information, vital information, and coach roster. All of this is surfaced in the portals using BDC.
6. Create an InfoPath form for the enrollment process. This includes member information and HRA information and uses InfoPath’s standard form validation.
7. Publish the InfoPath forms to the forms services for enabling the enrollment scenario.
8. Build audiences for members and coaches to support custom portals and personalization.
9. Assemble member portal with mandatory optional Web Parts.
10. Assemble coach portal with member roster and custom Web Parts.
11. Enable personalization for members and coaches.
A key architectural element of the member enrollment process is the integration with the Windows Live ID Identity Services (IDS) platform to provide identity services. The first step of this integration is the pre-registration with IDS through Microsoft Services Manager. Microsoft Services Manager is the central provisioning site for partners who integrate with Microsoft Web services for Live ID identity management. Microsoft Services Manager site is used for:
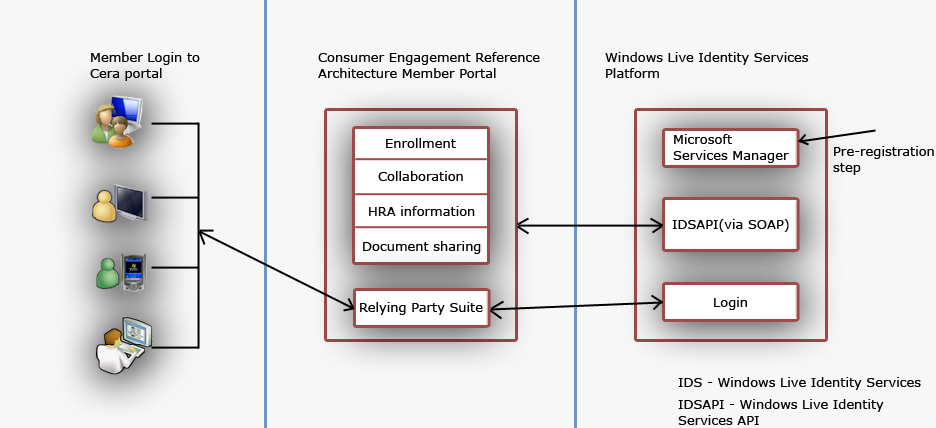
Figure 10. Integration with Windows Live ID
The provisioning process is presented as a workflow, which helps in determining the tasks that must be accomplished.
Member enrollment form
Once this step is completed successfully, then the next step is to setup the member enrollment form. CERA uses InfoPath to create the enrollment form and the HRA. It is easy to build InfoPath-based forms that generate healthcare standards–compliant XML. In addition, these forms are part of the familiar 2007 Microsoft Office Systems family of products and programming model.
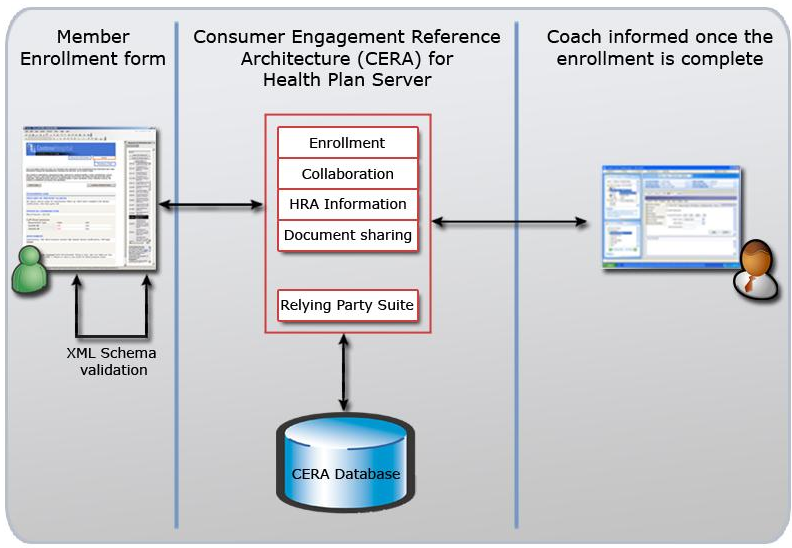
Figure 11. Enrollment process
As part of enrollment, members enter their personal information and HRA information. HRA information helps in creating a wellness profile to help coaches categorize the members and help them in reducing health risks. The HRA includes more than 50 questions related to member demographics, eating and exercise habits, and medical history. When members complete the HRA, their responses help in building a wellness profile that addresses many aspects of engagement with the members. Some of the key areas of using this information are to:
Figure 11 shows the flow when the member completes the enrollment form. Once the XML schema is validated, then the data is saved in the database and the coach is alerted about the new member.
HRA Validation
Once a member finishes the enrollment steps, the member is thanked for participating in the health plan through both the enrollment application and an e-mail. The member is also informed that they will receive a separate e-mail about the next steps, in case the member is completing the enrollment online. If the member is enrolling at a health fair, HRA validation happens immediately.
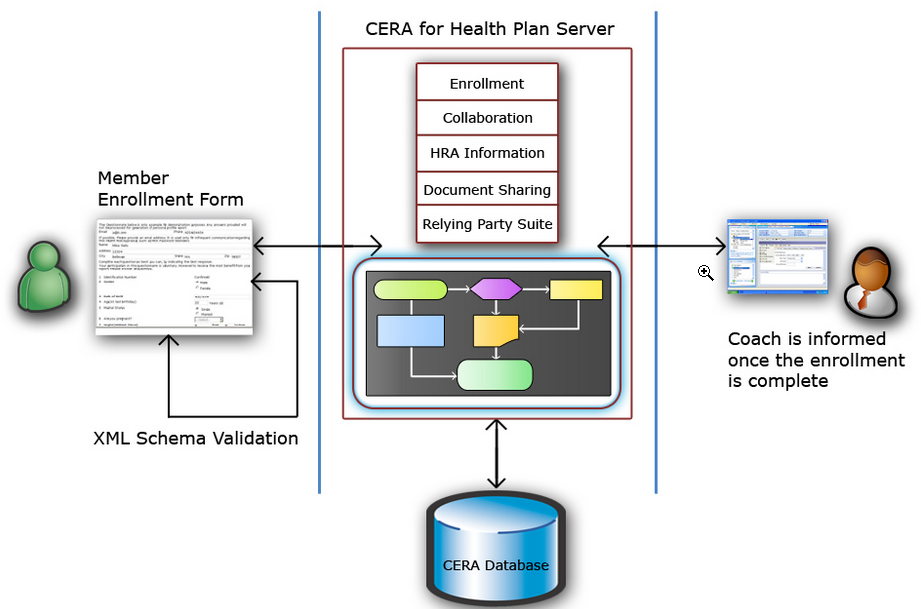
Figure 12. Enrollment completion triggers a workflow
In either case, once the member enrollment is completed, CERA triggers a workflow and adds the member enrollment form to the pending documents. At the same time, this new member is assigned to a coach.
Coach assignment can happen based on many different criteria. For example, the coach could be assigned based on,
CERA uses the simple method of round-robin to assign a member to a coach. Once a coach is assigned to the member, the coach receives an alert about the new member enrollment form.
HRA validation is done in person as it requires verification and validation of the member’s health risk. So the coach opens the enrollment form once the member is physically present for validation. Then the coach verifies the HRA in person by going over the member’s profile and health information such as weight, smoker/non-smoker. The coach draws blood for test, and so on. Finally, the coach updates the HRA information and completes the validation process. Once the validation process is completed, the member is successfully enrolled into the health and wellness coaching program.
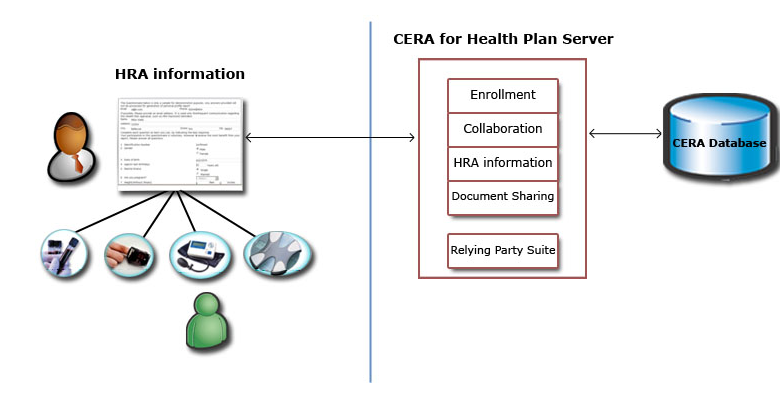
Figure 13. HRA validation
The coach then reviews the member profile and both assigns a priority based on the goals, motivation, health risk, and finally assigns the member to group of similar members, for example “smoking cessation” group or “weight loss” group.
Member portal
Once a member completes the HRA validation step, he/she is ready to receive coaching to improve overall health and wellness. The portal plays a critical role in collaboration with the coach to improve health. The member portal shows the member profile information and also health and wellness information. Different Web Parts display information surfaced from the database and other LOB applications.
The Business Data Catalog (BDC) is used extensively in CERA to surface information from the database and the LOB applications. Member health information, profile information, diagnostic information, lab results, and so forth are pulled into the portal using BDC.
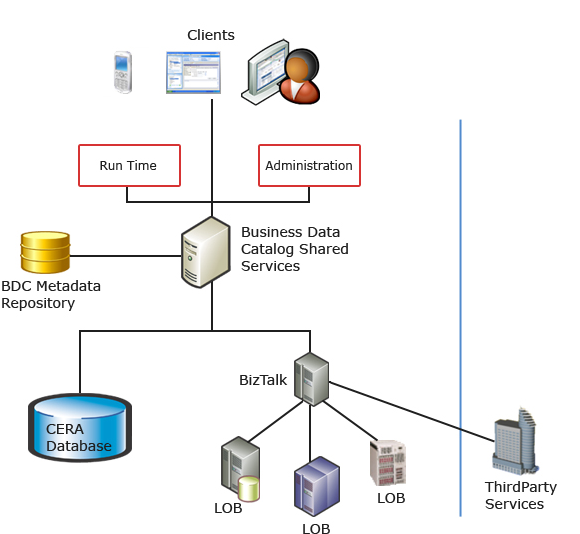
Figure 14. Surfacing information using BDC
As explained earlier, BDC is a metadata repository to define business entities stored in data. So it is used to define the entities for member profile information, vital information, and prescription information. It is also used to define entities for data from third-party applications such as lab testing applications, and disease management applications. This bridges the gap between the member portal site and the back-end databases and applications. This helps in bringing key data from various business applications to MOSS lists, Web Parts, search, user profiles, and custom applications.
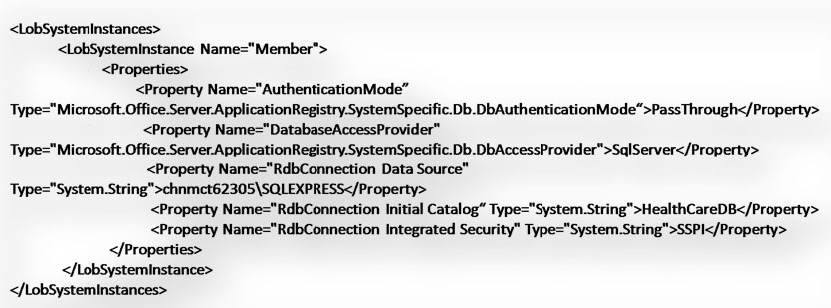
Figure 15. Sample BDC meta data
The above figure shows sample metadata for CERA with the authentication and connection string information to BDC. The metadata for CERA is manually defined, while the metadata for each data source is defined by identifying the business entities that member portal interacts with. In case of the CERA example, we defined the metadata for the member and activity entities methods that were used to fetch the data from the back-end server application.
This metadata model abstracts the underlying physical sources and provides a consistent and simple model for metadata authors working with different kinds of business applications.
Health Coach Portal architecture
A successful Health and Wellness Coaching program must enable Health Coaches to reach a large audience across an array of access channels. The two keys to a Health Coach’s success are his or her ability to economically scale across a large number of clients, and the ability to actively and positively change a member’s health and behavior.
To be economically successful, the Health Coach must use technology to scale across a large number of members. To successfully change the member’s health habits, the Health Coach must adapt to their environment and lifestyle to enable “moments of participation” across a myriad of devices. The Health Plan and the Health Coach must be able to electronically “go where consumers go” with direct-to-consumer connectivity and personal interactions within the context of the consumer’s daily life. Therefore, the consumer engagement reference architecture is a multi-channel platform that allows members to access their health and wellness information on any device, at any time, and from anywhere. This multi-channel flexibility enables the Health Plan and the Health Coaches to digitally insert themselves into the members’ lifestyle.
The 2007 Microsoft Office System combined with the .NET 3.0 frameworks provides the fundamental components required to support these needs.
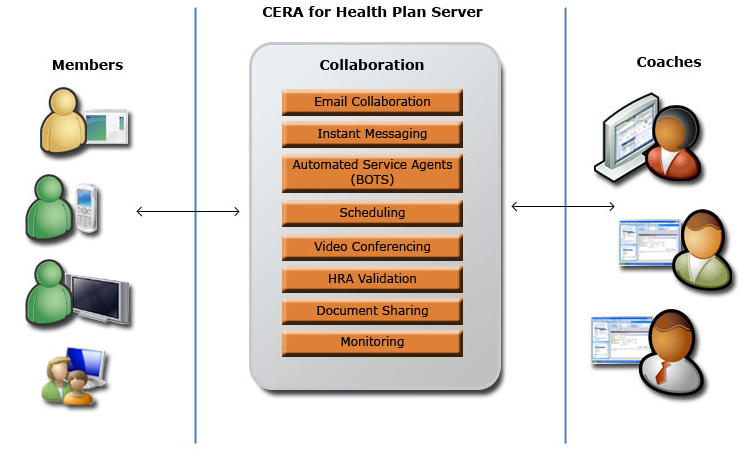
Figure 16. Collaboration
The workflow capabilities of MOSS play the critical role in improving the people collaboration in CERA. Engaging with the members triggers certain workflows for action on the coach’s part. For example when a member completes online enrollment, the enrollment InfoPath form triggers a workflow which leads to the assignment of a coach and a task is created for the coach. Workflow alerts the coach to take action on the member enrollment and setup a HRA validation appointment. Software can help in this step; however the most important process still depends on people. Automating interactions among the people who participate in the collaboration process can improve how that process functions, increasing its efficiency and lowering its error rate. Using software that supports human workflow can make organizations more effective.
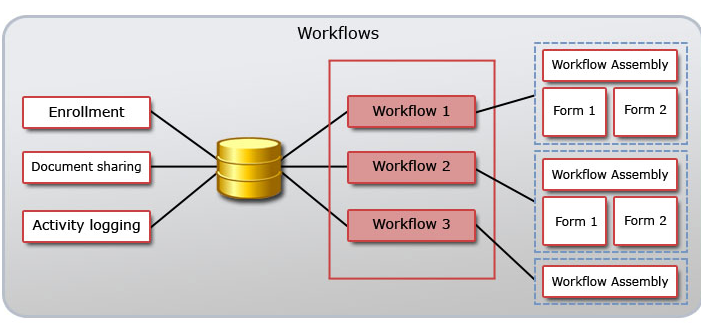
Figure 17. Workflows in CERA
Many kinds of collaboration processes in CERA benefit from automated support for human workflows. As shown above, the administrator of CERA can create a workflow library which consists of activities such as validate HRA information, activity logging approval, and so forth. In CERA these workflows were designed using the Visual Studio 2005 and Office SharePoint Designer. In both cases, the result is a workflow template that is deployed to the server.
Conclusion
In summary, Health care costs are rising rapidly and quality of care is suffering. Health plans need to think differently from the standard transactional systems they are used to for providing service. Health plans must engage consumers in their health planning and caring. However, there are many barriers to engage consumers, so the best solution is to go where consumers go using the vital consumer technologies such as online, media centers, and mobile devices.
The acute need for collaboration with consumers requires building a solution that can enable real-time collaboration that is contextual and meaningful. For this, it requires a platform that comes with certain capabilities to realize a solution quickly. Microsoft Office 2007 combined with .NET is one such platform to build a real-time collaboration solution to engage with consumers and improve quality of health while reducing the cost.